I was reading a fascinating study, which may completely change the way we approach pain management.
Typically when you have pain you reach for an anti-inflammatory drug. You keep taking those and eventually the body will heal itself and the pain will go away.
Or will it?
Why does some pain stay with us?
Researchers studied the mechanism for how acute pain becomes chronic or long-term pain. Acute pain is immediate pain. If unresolved, it becomes long-term or chronic pain. The researchers compared people with lower back pain who recovered from their injury to a second group whose lower back pain became chronic. They also confirmed the hypothesis using mouse models. Here’s what they discovered.
Working with your body’s natural immune response
The key difference observed in people whose acute lower back pain became long term back pain and those people who recovered from the back pain, came down to an immune cell called a neutrophil.
People with long-term pain had less neutrophils.
How your body responds to an injury
Your immediate reaction to an injury is to generate a vascular inflammatory response. Blood flows into the affected area bringing with it a whole host of cells really to begin the process of repair and healing. This is an immune response.
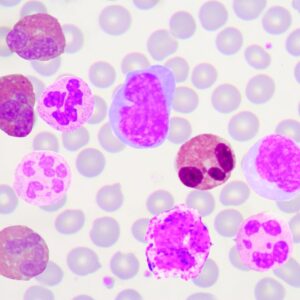
Some of these cells called cytokines, signal for other cells to join the party. Your cytokines alert chemokines. Your chemokines recruit leukocytes. A particular type of leukocyte is called a granulocyte. And they’re of interest because a neutrophil is a type of granulocyte.
What does a granulocyte do?
Granulocytes fight infections and allergens by dumping granules containing enzymes and chemicals into the affected area. Neutrophils are your first responders.
When your body detects bacteria or viruses it recruits granulocytes to ingest the bacterial microbes, destroying them with their own enzymes. This process is called phagocytosis.

You will notice this inflammatory process because your injured site will appear to be a bit redder in colour, or hot to touch, and there may be noticeable swelling and tenderness.
This phase typically lasts three to five days.
Once the damaged cells are tidied away, your body moves into the second phase, which is repair and regeneration.
How your body repairs an injury

In this second stage, your body lays down collagen fibres. Initiailly the rebuilding starts out in a disorganised, fragile manner.
This phase lasts between two days to eight weeks, depending on the extent of the injury. It’s really important to be gentle with yourself during this time as this is when you’re most susceptible to re-injuring the affected area.
Recovering from your injury
The final phase or phase three, is when remodelling and finalisation of your now improved structures takes place.The collagen fibres get organised and they now have stronger bonds between them.

You begin to be able to do more and to move more.
Stretching is really important during this phase as you want to maintain flexibility within the area.
Based on our understanding of these three stages of inflammation, what does this research suggest could be happening when we take an anti inflammatory, such as diclofenac?
How NSAIDs work
Non-steroidal anti inflammatory drugs or NSAIDs work by blocking the effect of those signalling chemicals. As a result, less inflammatory cells are recruited and the immediate pain subsides. But if we don’t have enough neutrophils on site, gobbling up microbes, we prolong the need for stage one of the inflammatory response.
As a result, once we stop taking our anti inflammatories, the pain associated with that much needed response returns. This creates a need for long-term pain relief and adds to the potential consequences of long-term systemic inflammation.
Pain killers vs Anti-inflammatories
You don’t have to suffer through an injury. It’s about allowing the inflammatory response to do its job. Painkillers or anodines can be used to manage the pain but choose those over an anti-inflammatory drug.

In episode 42, we talked about the benefits of contrast therapy, and how that can enhance the inflammatory process through the use of vasodilation and vasoconstriction.
Very little is known about why we sometimes have unresolved pain, and it can have a huge impact on our quality of life.
This study is an important step towards understanding not just for people living with pain or for doctors or pharmacists, but also for natural health practitioners, looking at herbs, food and movement that support our body through the inflammatory process. This could be the next generation and pain support and injury recovery.

