Did you know that between 2% and 10% of all prescribed drugs are non-steroidal anti-inflammatories, or NSAIDs? And that’s prescribed drugs. Many NSAIDs are available as over-the-counter medications, so they’re not counted in that prescribed drug count.
The journal US Pharmacist says that they account for around 60% of the analgesic market in the united states. Now there’s a place for NSAIDs, but with any drug, it’s helpful to know the pros and cons and to research the options, if you need to take NSAIDs over the longer term.
the first line of defence
They’re your first line of defence when it comes to inflammation, pain and fever. It’s helpful to know that while NSAIDs can reduce a fever, they don’t address the cause of the fever, which is usually viral or occasionally bacterial in nature and you need antivirals or antibiotics, depending on whether it’s a virus or a bacterial infection, to address the source of the fever.
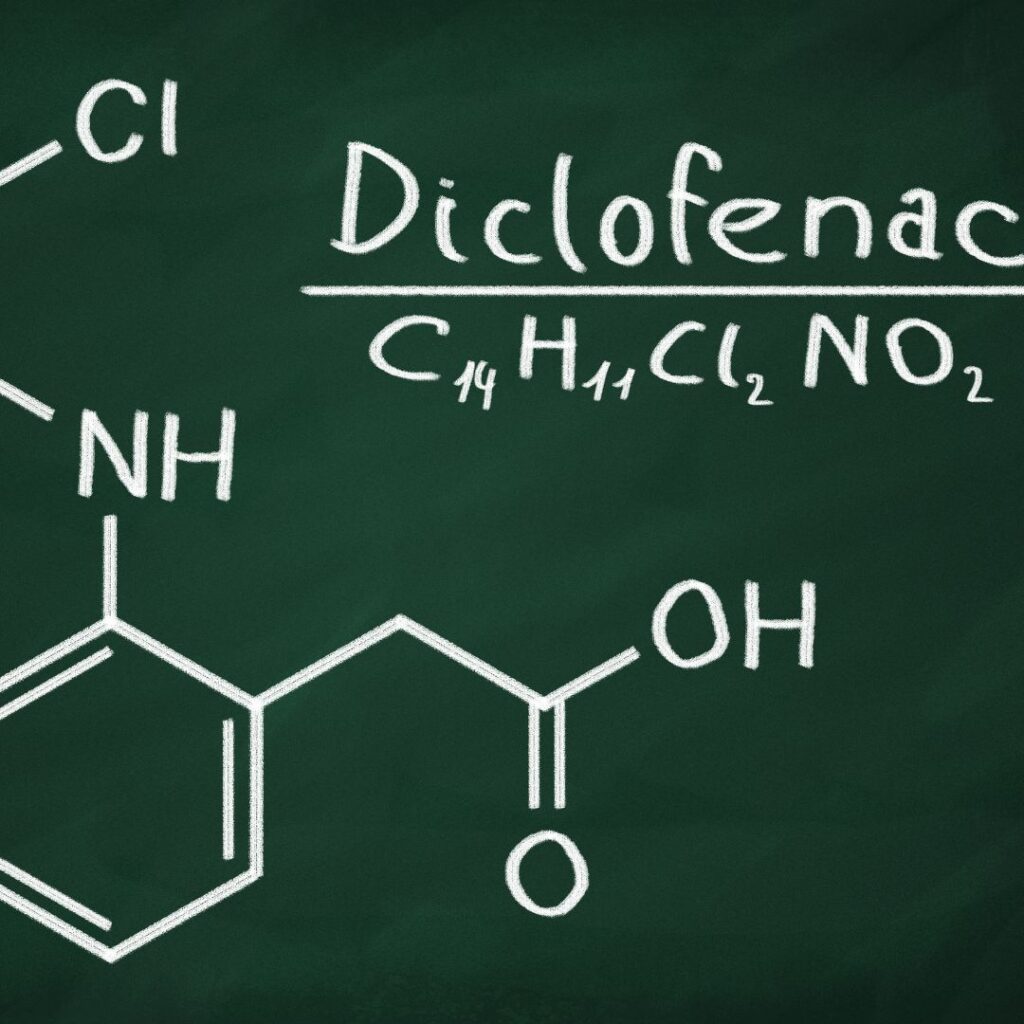
Common brands of nonsteroidal anti-inflammatory drugs include Ibuprofen and Diclofenac of which Voltaren is one brand name for Diclofenac, Naproxen and Ansaid, the brand name for flurbiprofen.
I mean, these researchers have a sense of humour, right, Flurbiprofen.
how do they work?
So, how do these drugs work? Well, our body responds to inflammation in a variety of ways. One of those ways involves activating an enzyme that’s known as cyclooxygenase. And we’ve got two types. Cyclooxygenase one and cyclooxygenase two or cox one and cox two for short. Cox one is involved in the physiological cascade that produces prostaglandins that are responsible for things like maintaining our kidney function or maintaining the protective mucosal layer in our gastrointestinal tract.

And it also is responsible for activating our platelets. Now we want our platelets to be activated when we injure ourselves because they’re involved in clotting. So very important. If you’re bleeding.
Cox two plays a key part in our body’s inflammatory response. It’s responsible for vasodilation, reducing or stopping the creation of platelets and the surge of smooth cells whose task it is to begin the repair process, an example of overenthusiastic repairing is atherosclerosis. Now, atherosclerosis describes that process where your arteries harden due to the plaque build up inside the artery.
Vasodilation is where your blood vessels widen to allow more blood to flush through, delivering all those lovely repair agents. It lowers blood pressure, and it floods the injury site with cells that are designed to stem the injury and begin the process of healing and repair. It’s why you get reddening and swelling at an injured site.
So, NSAIDs limit the activation of cox two, and as a result, we get a reduction in the associated pain, fever and inflammation. The problem is that some NSAIDs can’t differentiate between cox one and cox two, so they reduce the activity of both, and this results in an increased risk of gastrointestinal bleeding, and it stops the formation of that protective mucosal layer in your gut.

But, the challenge is that the research suggests that cox two selective NSAIDs may create a higher risk of cardiovascular events including stroke.
So, NSAIDs work, but the challenge is that using them over the long term or taking higher doses increases the risk of cardiovascular events, gastrointestinal, kidney or liver damage.
long term use of NSAIDs
Now, I’m not saying don’t take NSAIDs. I’m not saying that at all, they’re effective, and when it comes to low-grade pain management and reducing fever, they’re your first line of defence, but my suggestion is that if you’re relying on them.

But my suggestion is that if you are relying on them over the long term, work with a professional to see if you can find an alternative that either means you only take NSAIDs when the pain increases, and you need a short-term treatment boost to bring that pain back to manageable levels.
Work with a professional to potentiate the effect of NSAIDs so that you don’t need a higher dose. Now the interesting thing about herb, drug and supplemental food-drug interactions is that for the most part, we try to avoid them or minimise them, but in the hands of the right professional, you can use them to peak the treatment so that you need less of the drug to be effective.
Now, this isn’t something you have a go at. This is something where you work with a health care professional, such as a medical herbalist or a herb-trained pharmacist. The other option is to use NSAID alternatives when there’s a low-level injury, such as a sprain or a strain so that you’re reducing your overall consumption of NSAIDs.
managing acute pain
So, here are three options for managing acute pain caused by strains and sprains. First up, we’ve got arnica, now arnica is known botanically as arnica montana or Arnica Chamissonis and it originally hails from the mountainous regions of Europe all the way through to southern Russia. There are also arnica species that are native to northern America, which also have extensive traditional use.

Herbalists use the flower heads and we use the rhizome, but we only use it externally. The research has shown that the identified phytochemicals or plant chemicals within arnica are anti-inflammatory.
They’re a mild pain reliever. They’re antibacterial and antifungal, some research also shows that it has a small effect on reducing that platelet activity, so it’s often seen in creams for the treatment of sprains, strains and bruises.
The homoeopathic preparation is the one that’s taken internally, for topical applications, don’t use arnica if you’ve got dermatitis, or if the skin is broken, as in some cases, it can cause irritation. Now, there’s been extensive research on the pain-relieving properties of anica, particularly in relation to osteoarthritis and post-operative surgery. In relation to osteoarthritis, the majority of the reported research shows a significant reduction in pain scores and in relation to pain management following surgery, it’s a modest decrease in pain, which was also reported, but the research also showed that arnica was better tolerated than pain medications such as diclofenac. So, tell me, do you like chillies?

I’m talking about the real hot stuff. If chilli is something that you can happily tolerate, then hot peppers such as cayenne, jalapeno and the chilli pepper may be a useful, pain-relieving agent for you.
Something good to add to your diet. Cayenne stimulates your digestion, and interestingly, it’s also a carminative. Carminatives discretely move gas out of your system so they’re really helpful when you’ve overindulged or you’ve eaten something you’re sensitive to or you have bloating, but in terms of relieving neuralgia or nerve-based pain and other pain conditions, it’s all about capsaicin.

Capsaicin is what gives your chilli its pungent heat. Research shows an external application of capsaicin can help to manage skin disorders, shingles, muscle strain, arthritis-related disorders, diabetic neuropathy and other pain disorders, it’s quite extensive.
Capsaicin has also been studied for its ability to act as an anti-microbial and antiviral. Now, in relation to reducing pain, capsaicin connects with a t-cell receptor known as trpv1, and by doing this, the receptor gets a bit worn out, and as a result it becomes desensitised and the pain signalling is paused.
The effectiveness of capsaicin comes down to dose, with low-dose products showing limited effectiveness, and there’s been extensive research, including a Cochrane review in 2013, which suggests that an 8% topical capsaicin concentration is the most effective. Now, if the hot stuff isn’t for you, that’s ok, try pineapple.

Bromelain is an enzyme that’s extracted from the stem and the juice of the pineapple. Research reports it’s anti-inflammatory, and it is a pain reliever, particularly in relation to arthritic conditions. It also reduces swelling.
Trials assessing bromelain in osteoarthritis have used doses of bromelain in the range of 540 to 1890 milligrams a day, but, the higher doses of around 945 milligrams and up have caused gastrointestinal upset, such as diarrhoea, nausea and gas in some people.
So this is one to start on a lower dose and then build up as you need, depending on how your body responds to it. The research shows that a therapeutic benefit has been observed at 160 milligrams a day, so you’ve got a lot of flexibility there. Now, you need to eat a lot of pineapples to get an effective dose, and that’s not great if you’re diabetic with all that sugar, so this one is better as a supplement.
review your intake
If you’re wondering about your current intake of NSAIDs, get a medication review by talking to your pharmacist or your doctor. Research the pros and cons of the supplements that we’ve talked about today. And if you’re taking any type of medication, have a conversation with a health professional, such as a medical if you’re taking any type of medication, have a conversation with a health professional such as a medical herbalist, pharmacist or doctor, so that you’re aware of any possible interactions

